Other Methods
Plan B®
Plan B® is a pill that is intended to be used after unprotected intercourse. Each Plan B® tablet contains 0.75 mg of a single steroid called Levonorgestrel.
How it works:
- Prevents implantation of a human embryo by thinning the lining of the uterus and making it more slippery.
- Preventing ovulation (by altering tubal transport of sperm and/or ova.)
Plan B® is not recommended for routine use as a birth control pill. In studies, 12% of women bled more than usual after use of Plan B®.
Birth Control Implant
A Birth Control Implant is a stick-like medical device that is 1 ½ inches long (4cm) and is inserted under the skin in a woman’s arm. It contains birth control hormone chemicals.
How it works:
- Prevents implantation of a fertilized egg by thinning the lining of the uterus and making it more slippery.
- Inhibits ovulation.
- Increases cervical mucus to inhibit sperm from reaching the egg.
An implant should not be used if the woman has had blood clots, or unexplained vaginal bleeding. If one decides to remove the implant, surgery in the hospital may be needed. If women are diabetic, have high cholesterol, headaches, kidney problems, high blood pressure, or get depressed, they should first consult with their doctor before getting an implant.
Birth Control Shots
Birth Control Shots contains a birth control hormone chemical. The shot is also known as Depo-Provera. The drug is Medroxyprogesterone which is a form of progesterone, a female hormone.
How it works:
- Prevents implantation of a fertilized egg by thinning the lining of the uterus and making it more slippery.
- Inhibits ovulation.
- Increases cervical mucus to inhibit sperm from reaching the egg.
Call your doctor at once if you have any of these serious side effects from the shot:
- menstrual periods that are heavier or longer than normal;
- sudden numbness or weakness, especially on one side of the body;
- sudden severe headache, confusion, problems with vision, speech, or balance;
- chest pain, sudden cough, wheezing, rapid breathing, coughing up blood;
- pain, swelling, warmth, or redness in one or both legs;
- fever;
- nausea, upper stomach pain, itching, loss of appetite, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes);
- swelling in your hands, ankles, or feet; or
- symptoms of depression (sleep problems, weakness, mood changes).
Less serious side effects may include:
- changes in your menstrual periods;
- weight gain;
- mild headache, drowsiness;
- mild stomach pain;
- hot flashes;
- joint pain;
- breast tenderness;
- feeling tired or irritable;
- acne;
- decreased sex drive; or
- skin changes or a hard lump where the injection was given.
Critical Side Effects of Depo Provera
Depo-Provera has the following critical side effects on its users:
- Breast Cancer: According to three separate studies, breast cancer occurs two to four times more often among young women who use Depo-Provera.
- Osteoporosis: Depo-Provera is now believed to cause loss of bone mass among women. Osteoporosis is a debilitating condition that becomes more life-threatening as women grow older.
- Cervical Cancer: Some studies indicate that Depo-Provera increases the risk of cervical cancer.
- Excessive Bleeding: Depo-Provera can cause heavy and prolonged menstrual bleeding.
- Weight Change: On average, Depo users gain 12-16 pounds over four to five years, but some women have gained up to 40 pounds.
- Difficulty Getting Pregnant: Some women who stop using Depo-Provera don’t get their period again for as long as two years, preventing pregnancy for much longer than intended.
- HIV, Chlamydia, & Gonorrhea: Recent studies have shown that women using Depo have an increased risk of contracting HIV, chlamydia, and gonorrhea
- Other Side Effects: Severe Depression, Loss of Sex Drive, Fatigue, Dizziness, Headaches, Nervousness, Abdominal Pain, Hair Loss, Facial Hair Growth
The Patch (Ortho Evra):
The patch is placed on your body and it contains hormones (norelgestromin and ethinyl estradiol). It sticks to your skin and over time, releases the hormones.
How it works:
- Prevents implantation of a fertilized egg by thinning the lining of the uterus and making it more slippery.
- Inhibits ovulation.
- Increases cervical mucus to inhibit sperm from reaching the egg.
The patch contains 60% more estrogen than the pill and may cause blood clots leading to a stroke or heart attack resulting in death or disability.
For more information, click on: The Patch
Nuva Ring:
Nuva Ring is a vaginal ring that contains the hormones estrogen and progestin.
How it works:
- Prevents implantation of a fertilized egg by thinning the lining of the uterus and making it more slippery.
- Inhibits ovulation.
- Increases cervical mucus to inhibit sperm from reaching the egg.
The woman inserts the ring into her vagina and wears it for 3 weeks per month. Nuva Ring may cause blood clots, stroke or heart attack.
For more information, click on: Nuva Ring
Diaphragm Birth Control:
A diaphragm is a circular cup that is placed in the vagina prior to intercourse. Most women also put about a table spoon of spermicide in the cup to avoid pregnancy. There are different size diaphragms from 2 to 4 inches in diameter. Your health care provider can help you determine the appropriate size. It is designed to cover the cervix in order to prevent sperm from entering the uterus. The diaphragm should not be removed until 6 hours after intercourse, but should be removed within 24 hours.
Essure™:
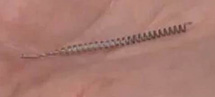 Essure™ is a device made of a nickel titanium alloy that is inserted into both fallopian tubes in an effort to block them so that the sperm does not reach a woman’s ova (egg). It is inserted by a doctor at his/her office. The manufacturer indicates that Essure™ has some risks. During the procedure to insert them, part of the device may break off and puncture the fallopian tube. In rare instances, the device may migrate into the lower abdomen and pelvis.
Essure™ is a device made of a nickel titanium alloy that is inserted into both fallopian tubes in an effort to block them so that the sperm does not reach a woman’s ova (egg). It is inserted by a doctor at his/her office. The manufacturer indicates that Essure™ has some risks. During the procedure to insert them, part of the device may break off and puncture the fallopian tube. In rare instances, the device may migrate into the lower abdomen and pelvis.
Essure Birth Control to be Taken Off Market
Vasectomy
A vasectomy is a minor surgical process for the man. It is permanent birth control and is used after a person has decided to no longer have children. A vasectomy will not interfere with the man’s sex drive, ability to have erections, sensation of orgasm, or ability to ejaculate. Semen or fluid, will still be produced and ejaculated during sex but will no longer contain sperm. It will only contain fluids that are produced by the male reproductive system.
Most of the fluid in semen is produced by the prostate gland. That fluid will continue to be produced and during sex will be ejaculated. The sperm however is produced in the testicles and therefore during a Vasectomy the small tubes leading from the testicles to the prostate are clamped, closed, or cut to prevent the sperm from getting there. The sperm is then simply absorbed in the man’s body, but the semen fluid is still ejaculated during sex. The name of the tube that is cut is “Vas deferens.” The anatomy is illustrated in a drawing on the following webpage: http://www.webmd.com/men/male-reproductive-system
A vasectomy can be done in a doctor’s office during a 30 minute procedure. A local anesthetic is used to minimize discomfort during the procedure. In about one week, or whenever the man is comfortable, sexual activity can resume, although it will take six weeks before the sperm is no longer in the upper part of the tube. A Vasectomy is nearly 100% effective in preventing pregnancy. A graphic video that shows the procedure (the most popular vasectomy video – having been viewed by over 800,000 people) is at the following link: https://www.youtube.com/watch?v=uwjL2F-kG7s
With this birth control method the man’s partner does not have to use birth control pills that introduce chemicals into her body on a repeated basis. Also, it will not result is a little human life being conceived, therefore the risk of abortion is not present.
Tubal Ligation
After deciding that she doesn’t want any more children, a woman may choose Tubal Ligation as means of permanent birth control. Sometimes called, “getting her tubes tied,” a tubal ligation is surgical procedure in which a doctor will cut, tie (ligate), or clamp shut the fallopian tubes. This prevents an ovum (or egg) from moving from the ovaries and through the fallopian tubes. A tubal ligation is sometimes done after a woman has had a c-section (and the baby has been born) since a surgery in already in process and the woman desires to have no further children. Tubal Ligation is nearly 100% effective in preventing pregnancy.
Tubal Ligation is considered major surgery and is done under general anesthesia in an operating room. One way of doing a tubal ligation is laparoscopicaly, that is, using a telescope-like instrument. Using this method the doctor makes two small incisions in the abdomen and can see with a video-like camera. It is called Laparoscopic Bi-Lateral (both sides) Tubal Ligation. Here’s a description of the steps:
- The woman receives general anesthesia.
- An instrument is inserted through the vagina to move the uterus into position during the operation.
- A small incision is made at the navel (belly button).
- Gas is introduced to distend (expand) the woman’s abdomen.
- A laparoscope is inserted through the incision.
- Another small incision is made in the lower abdomen to insert a surgical instrument.
- Clips are applied to the fallopian tubes.
With this birth control method a woman does not have to use birth control pills that introduce chemicals into her body on a repeated basis. Also, it will not result is a little human life being conceived, therefore the risk of abortion is not present.
For a diagram showing an illustration of a tubal ligation, click: http://www.mayoclinic.org/tests-procedures/tubal-ligation/multimedia/tubal-ligation/img-20006963
For a graphic video showing a Laparoscopic Bi-Lateral Tubal Ligation, click on: http://www.youtube.com/watch?v=M8sXvBptUCM
Note: Information on this website is intended to supplement, not substitute for the knowledge of your doctor, or other health care provider.

