Full Academic Article
Postfertilization Effects of Oral Contraceptives and Their Relationship to Informed Consent
Walter L. Larimore, MD; Joseph B. Stanford, MD, MSPH
Arch Fam Med. 2000;9:126-133
Oral contraceptives (OCs) are among the most extensively studied and used medications in the world,*1 and are accessible without a prescription in some countries, although still virtually unavailable in others. In America, OCs have contributed to an increased acceptability of birth control,2 although, for many patients, decisions about contraception still have moral, ethical, and religious implications.3, 4 For patients who believe that human life begins at fertilization (conception), a method of birth control that has the potential of interrupting development after fertilization (a postfertilization effect) may not be acceptable.5, 6 Postfertilization effects are operative for emergency (postcoital) contraception (when it is administered too late to prevent ovulation),7, 8 luteolytic agents (ie, RU-486),9 and intrauterine devices,5 and these methods therefore are unacceptable to some patients. Although postfertilization effects have been cited as a secondary mechanism of OCs,10-12 the evidence for such effects has not been systematically reviewed. The purpose of this article was to review and grade the available evidence for postfertilization effects of OCs and discuss the implications for informed consent, based on the premise that patients to whom postfertilization effects are important have the right to make decisions based on the best available evidence.13-15
Our analysis of the evidence involved a review of the abstracts of all studies of OCs published since 1970 available on MEDLINE that discussed the commonly used OCs, including low-dose (<50 µg of estrogen) phasic combined oral contraceptives (COCs), low-dose monophasic COCs, and progestin-only OCs (progestin-only pills [POPs]). We also reviewed the patient handouts provided by OC manufacturers and the most recent editions of several medical textbooks and reference books.
Since there is variability in the definitions and use of terminology in reproductive medicine, we used the American Academy of Obstetrics and Gynecology Committee on Ethics’ definitions for fertilization, implantation,embryo, and preembryo.16 Preembryo is a general term that includes the human developmental stages that occur after fertilization but prior to the appearance of the primitive streak about 14 days after fertilization. From that point until the end of the eighth week after fertilization, the term embryo is used. Implantation is the process whereby the preembryo attaches to the endometrial lining of the uterus. This process begins 5 to 7 days after fertilization and may last several days. For this review, we defined postfertilization effects to include mechanisms of action that operate after fertilization to prevent a clinically recognized intrauterine pregnancy. We looked specifically for studies referencing any postfertilization effects of OCs. When many studies indicated similar findings, we listed the most recent or most methodologically sound references or other systematic or general reviews of particular subjects.
MECHANISMS OF OCs
The literature discusses several mechanisms for OCs. While the primary effect of OCs is the inhibition of ovulation via suppression of pituitary gonadotropin secretion (this mechanism is operative most of the time),1,10, 12 secondary effects are implicated at times of breakthrough ovulation to prevent clinically recognized pregnancy.17, 18 We classified these secondary effects as occurring either prefertilization or postfertilization. Secondary prefertilization effects may include alterations in cervical mucus that limit sperm penetration2, 17-20 and changes in the endometrium and fallopian tube that may impede normal sperm transport.2, 17, 18, 21
Breakthrough ovulation rates vary by the form and the dose of the OC used.2, 10, 12, 18, 22 With OCs, breakthrough ovulation is more likely with lower doses of estrogen and with imperfect rather than perfect use.10, 12,16, 17, 23-25 Perfect use of OCs implies taking them consistently and correctly (ie, in the correct order, on time, each and every day, and without other medications that might diminish the effectiveness of OCs). Typical use is described as the full range of usage patterns for OCs that actually occur in women.1, 11, 12, 18 While some smaller studies that evaluated small numbers of women for 6 or fewer cycles have reported breakthrough ovulation rates of near 0, studies that evaluated women for at least 6 cycles demonstrated ovulation rates ranging from 1.7%25 to 28.6%23 per cycle. For POPs, reported breakthrough ovulation rates range from 33%26 to 65%.20, 27, 28
Obviously, breakthrough ovulation can result in unintended pregnancy1, 17, 18; however, the pregnancy rates with typical use vary widely and are often underestimated.29 Unadjusted analyses of unintended pregnancies while using COCs report rates of 0.1 to 1.0 per 100 woman-years of use in perfect use and 3 per 100 woman-years in the first year of typical use.1, 10, 12, 17, 18, 20 Most of these data do not account for elective abortions. One national analysis that accounted for the underreporting of elective abortions estimated that the unintended pregnancy rates during the first year of OC use were 4% for “good compliers,” 8% for “poor compliers,” and up to 29% for some users.29 Rates of pregnancy are higher with POPs than with COCs.1, 17, 18 Unadjusted analyses of pregnancies while taking POPs reported rates of 0.5 to 1.0 per 100 woman-years of perfect use and 3 to 7 per 100 woman-years in the first year of typical use.1, 10, 12, 17, 18, 20 However, these rates have not been adjusted for elective abortions and are almost certainly underestimated.29Progestin-only pills are reported to have potent effects on both cervical mucus and the endometrium.19-21, 30, 31 While this has led to speculation that “the principal mode of action is . . . to make the cervical mucus hostile to the transport of the sperm,”17 animal model data32 and data on ectopic pregnancy rates (reviewed below) suggest that postfertilization effects also play a role.
In theory, postfertilization effects of OCs could involve any 1 or more of the following 3 mechanisms of action: (1) A postfertilization preimplantation effect would consist of a slower transport of the preembryo through the fallopian tube, preventing the preembryo from implanting in the uterus; this could result either in the unrecognized loss of the preembryo or in an ectopic (tubal) pregnancy if the preembryo had slower tubal transport and ended up implanting in the fallopian tube. (2) A peri-implantation effect would be the alteration of the endometrium, such that a preembryo that reached the uterus was unable to successfully implant into the endometrial lining of the uterus. (3) A postimplantation effect could result from alteration of the endometrium not sufficient to prevent implantation but unfavorable for maintenance of the pregnancy; a preembryo or embryo already implanted in the endometrial lining of the uterus would be unable to maintain itself long enough to result in a clinically recognized pregnancy.
EVIDENCE FOR POSTFERTILIZATION EFFECTS
Direct evidence of postfertilization preimplantation and peri-implantation effects would require methods that directly measured the rate of fertilization and the loss of the preembryo in women taking OCs. Transcervical tubal washings have been used in women using intrauterine devices to quantify the rate of ova fertilization33 and could theoretically be done for women taking OCs. However, there is no proven method to measure the loss of the preembryo prior to implantation, even though a number of possible methods have been investigated that involve maternal hormones that may be produced or altered after fertilization.34-36 Probably the most promising method is the isolation of “early pregnancy factor.”37-39
Direct evidence of a postimplantation effect on the preembryo or embryo prior to clinically recognized pregnancy would require measurement with ultrasensitive assays for β–human chorionic gonadotropin (β-HCG) or other pregnancy-related hormones.40 Although ultrasensitive assays for β-HCG have been done with normally fertile women not using OCs,41-44 as well as with women using nonhormonal methods of contraception,45we could find no such studies in women using OCs. Despite the lack of these data, at least 3 lines of evidence have been suggested to support the hypothesis that 1 or more postfertilization effects are operative in at least some women taking OCs. Using a standard quality of evidence table46 (Table 1), we graded the available evidence.
Endometrial Changes That May Affect Endometrial Receptivity
Oral contraceptives directly affect the endometrium.1, 10, 12, 20, 21 These effects have been presumed to render the endometrium relatively inhospitable to implantation or to the maintenance of the preembryo or embryo prior to clinically recognized pregnancy by producing a predecidual or decidualized endometrial bed with diminished thickness and with widely spaced, exhausted, and atrophied glands; by altering the cellular structure of the endometrium, leading to the production of areas of edema alternating with areas of dense cellularity18, 20, 21; and by altering the biochemical and protein composition of the endometrium.47 Although these changes are consistently seen in women taking OCs, there is currently no direct evidence to link these changes to preembryo or embryo loss in women taking OCs. However, this hypothesized postfertilization effect seems to be so well accepted that in many medical articles and textbooks it has been explicitly listed as the third mechanism of OCs (after suppressing ovulation and prefertilization effects).1, 10,17, 18 For example, the Food and Drug Administration–approved product information for OCs in the Physicians’ Desk Reference states,
Although the primary mechanism of this action is inhibition of ovulation, other alterations include changes in the cervical mucus, which increase the difficulty of sperm entry into the uterus, and changes in the endometrium, which reduce the likelihood of implantation.11
An independent clinical pharmaceutical reference also contains this assertion.12 We considered this level III (poor to good) evidence (Table 1).
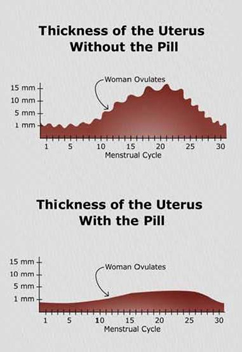
To assess the clinical significance of an altered endometrium, it was helpful to examine data that compared endometrial thickness with the receptivity of the endometrium to preembryos during in vitro fertilization procedures. Magnetic resonance imaging scans of the uteri of women reveal that the OC users have endometrial linings that are consistently thinner than the endometrial linings of nonusers,48-50 up to 58% thinner.51Of the first 4 ultrasound studies published, the first did not find a relationship between endometrial thickness and in vitro fertilization implantation rates52; however, subsequent studies noted a trend,53, 54 and one demonstrated that a decreased thickness of the endometrium decreased the likelihood of implantation.55 Larger, more recent, and more technically sophisticated studies56-65 all concluded that endometrial thickness is related to the functional receptivity of the endometrium. Furthermore, when the endometrial lining becomes too thin, then implantation does not occur.56-58, 64, 65 The minimal endometrial thickness required to maintain a pregnancy in patients undergoing in vitro fertilization has been reported, ranging from 5 mm55 to 9 mm65 to 13 mm,53 whereas the average endometrial thickness in women taking OCs is 1.1 mm.50 These data would seem to lend credence to the Food and Drug Administration–approved statements that ” . . . changes in the endometrium . . . reduce the likelihood of implantation.”11 We considered this level II.2 (good to very good) evidence (Table 1).
Integrin Changes Affecting Fallopial Tube and Endometrial Receptivity for Implantation
Integrins are a family of cell adhesion molecules that are accepted as markers of uterine receptivity for implantation.66, 67 Temporal and spatial expression of these endometrial peptides is believed to contribute to the establishment and maintenance of a cyclical endometrial receptivity. Three cycle-dependent integrins (α1β1, α4β1, αVβ3) have been shown to be ” . . . coexpressed apparently only for a brief interval of the cycle that corresponds with the putative window of maximal uterine receptivity” and ” . . . have emerged as reliable markers of normal fertility.”68 Of these 3, the αVβ3 integrin seems “to be an excellent marker to study the molecular events leading to the establishment of uterine receptivity and successful implantation.”68, 69 These 3 integrins are conspicuously absent in the endometrium of most patients with luteal phase deficiency, endometriosis, and unexplained infertility.68
In addition, integrin expression is significantly changed by OCs. Integrins have been compared using endometrial biopsy specimens from normally cycling women and women taking OCs. In most OC users, the normal patterns of expression of the integrins are grossly altered, leading Somkuti et al68 to conclude that the OC-induced integrin changes observed in the endometrium have functional significance and provide evidence that reduced endometrial receptivity does indeed contribute to the contraceptive efficacy of OCs. They hypothesized that the sex steroids in OCs alter the expression of these integrins through cytokines and therefore predispose to failure of implantation or loss of the preembryo or embryo after implantation. We considered this level II.3 (good) evidence (Table 1).
Integrins have also been identified in the fallopian tube.69 Of interest, the αV subunit is expressed in the fallopian tube epithelium throughout the cycle, but the β3 subunit is only upregulated during the period of endometrial receptivity. Therefore, it has now been postulated that the normal tubal epithelium also has an implantation window that ” . . . affords the opportunity for trophoblast attachment should a 5-7 day preembryo be unduly retained in the tube.”69 As discussed earlier, one of the postulated actions of the OCs is a slowing of tubal peristalsis (via smooth muscle relaxation)70; therefore, a reduction in tubal peristalsis that is associated with an upregulation of the αVβ3 integrin in the epithelium of the fallopian tube could theoretically lead to an increased risk of ectopic pregnancies in women taking OCs.
If breakthrough ovulation occurs while using the COC, then to some extent ovarian and blastocyst steroidogenesis could theoretically “turn on” the endometrium, causing it to normalize prior to implantation in the ovulatory cycle. However, after discontinuing use of COCs, it usually takes several cycles for a woman’s menstrual flow to approach the volume of women who have not taken hormonal contraception,71 suggesting that the endometrium is slow to recover from its COC-induced atrophy. Furthermore, in women who have ovulated secondary to missing 2 low-dose COCs, the endometrium in the luteal phase of the ovulatory cycle has been found to be nonsecretory.23
Increased Extrauterine Pregnancy to Intrauterine Pregnancy Ratio
If the action(s) of OCs on the fallopian tube and endometrium were such as to have no postfertilization effects, then the reduction in the rate of intrauterine pregnancies in women taking OCs should be proportional to the reduction in the rate of extrauterine pregnancies in women taking OCs. If the effect of OCs is to increase the extrauterine-to-intrauterine pregnancy ratio, this would indicate that one or more postfertilization effects are operating. All published data that we could review indicated that the ratio of extrauterine-to-intrauterine pregnancies is increased for women taking OCs and exceeds that expected among control groups of pregnant women not currently using OCs. These case-controlled series come from 33 centers in 17 countries and include more than 2800 cases and controls.72-77 The odds ratios in these studies ranged from 1.7 (95% confidence interval [CI], 1.1-2.5)72 to 1.8 (95% CI, 0.9-3.4)73 to 4.3 (95% CI, 1.5-12.6)74 to 4.5 (95% CI, 2.1-9.6)75 to 13.9 (95% CI, 1.8-108.3).76 The letter by Job-Spira et al74 seems to represent the same data set of 279 cases and controls as the study by Coste et al.76 The meta-analysis by Mol et al73 includes 2 of the publications,72, 75 but one of these may include women taking POPs.72 Therefore, of the 5 publications, only 2 allow review of the association of COCs with ectopic pregnancy.75, 76 These 2 studies from 7 maternity hospitals in Paris, France, and 3 in Sweden involved 484 women with ectopic pregnancies and 289 pregnant controls and suggest that at least some protection against intrauterine pregnancy is provided via postfertilization preimplantation effects. We recognize that studies that have used nonpregnant controls have not shown a risk of increased ectopic pregnancy for users of COCs. In our review, we restricted our analysis to studies using pregnant controls, because we concur with researchers73, 76 in this field that ” . . . when considering the situation where a woman became pregnant during contraceptive use, one should focus on pregnant controls.”73 Therefore, COC use seems to be associated with an increased risk of ectopic implantation or unrecognized loss of preembryos. We considered this level II.2 (good to very good) evidence (Table 1).
Ectopic pregnancy is a particular form of postfertilization loss that involves substantial risks to the woman, and thus the absolute risk of ectopic pregnancy for women taking OCs will be of interest to clinicians and patients. Converting a relative risk of ectopic pregnancy to an absolute risk has many inherent difficulties that have been reviewed elsewhere.78 Nevertheless, adapting the method suggested by Franks et al78 would allow one to predict that the ectopic pregnancy rate for women taking OCs would be the product of 3 factors: (1) the overall pregnancy rate per 1000 woman-years among those taking OCs, (2) the proportion of extrauterine pregnancies compared with all pregnancies for a comparable control population not taking OCs, and (3) the relative risk for ectopic pregnancy in women taking OCs compared with the control population, which may be estimated by the odds ratio from case-control studies. For factor 1, Potter29 suggests 40 for good compliers and 80 for poor compliers. For factor 2, the proportion of ectopic pregnancies in the 1990s is estimated to range from 1 in every 5679 to 6480, 81 pregnancies (0.0156 to 0.0179). A reasonable range for factor 3 would be 1.1 to 13.9, based on the studies discussed above. This model would predict an absolute risk ranging from 0.7 (40 X 0.0156 X 1.1) to 19.9 (80 X 0.0179 X 13.9) ectopic pregnancies per 1000 woman-years. We could only find one study, from Zimbabwe, which reported an absolute risk of ectopic pregnancy in women taking OCs of 0.582 per 1000 woman-years.
The risk of ectopic pregnancy is higher with POPs, and ectopic pregnancy has been discussed at length by a number of investigators as a clinically significant potential complication of POPs.82-84 The odds ratio of an extrauterine pregnancy for a woman taking a POP (compared with pregnant controls) was reported in only one study and was 79.1 (95% CI, 8.5-735.1).74 Assuming an overall clinical pregnancy rate of 30 to 70 per 1000 woman-years, this equates to a predicted absolute risk of 4 to 99 ectopic pregnancies per 1000 woman-years ([30 or 70] X [0.0156 or 0.0179] X [8.5 or 79.1]) in women taking POPs. This is reasonably concordant with absolute rates of ectopic pregnancy in women taking POPs, which have been reported to range from about 382, 83, 85 to about 2084, 86 per 1000 woman-years.
Data from case-controlled series demonstrate that women with clinically recognized pregnancy are no more or less likely to miscarry based on whether they were taking an OC after their pregnancy was clinically recognized.87-90 However, the epidemiology, biology, and recognized risk factors of clinically recognized embryo or fetal loss (spontaneous abortion after clinically recognized pregnancy) do not seem to apply to early (unrecognized) preembryo or embryo loss, as the available evidence suggests that the mechanisms of early establishment and maintenance of pregnancy and later maintenance of pregnancy are qualitatively and substantially different.90
COMMENT
We found the evidence supporting postfertilization effects for OCs in the prevention of clinically recognized pregnancy to range from poor (level III) to very good (level II.2). Specifically, evidence based on alterations in endometrial biochemistry and histology (level III), evidence based on endometrial thickness and endometrial receptivity from research studying in vitro fertilization (level II.2), and evidence based on endometrial integrins (level II.3) all support the possibility of peri-implantation or postimplantation effects. Furthermore, evidence based on ectopic-to-intrauterine risk ratios from multiple case-control studies (level II.2) supports the possibility of postfertilization preimplantation, peri-implantation, or postimplantation effects. However, we could identify few data that would assist in quantifying these postfertilization effects. It seems likely that for perfect use of COCs, postfertilization mechanisms would be likely to have a small but not negligible role. For POPs, COCs with lower doses of estrogen, and imperfect use of any OCs, postfertilization effects are likely to have an increased role. In any case, the medical literature does not support the hypothesis that postfertilization effects of OCs do not exist.
Despite the evidence, which suggests that postfertilization effects for OCs are operational at least some of the time, and the fact that a postfertilization mechanism for OCs is described in the Physicians’ Desk Reference,11 in Drug Facts and Comparisons,12 and in most standard gynecologic, family practice, nursing, and public health textbooks, we anecdotally find that few physicians or patients are aware of this possibility. Therefore, we believe that the potential for postfertilization effects is probably not routinely presented to patients as part of their informed consent to use an OC. Furthermore, it is of concern to us that only one of the many OC patient information handouts we and others5 have reviewed, including those produced by the OC manufacturers, mentions the possible postfertilization mechanism, despite the fact that this information is nearly always included in the professional labeling of these same OCs.
Since there is evidence to support the existence of postfertilization effects and because it is impossible to know in advance which patients would find the potential for this effect objectionable, we believe that the lack of information regarding postfertilization effects in patient information materials about OCs represents a potential failure to provide complete informed consent. Furthermore, if this mechanism of an OC violates the moral requirements of a woman, then failure to disclose this information seriously jeopardizes her autonomy. If information about the mechanism of an OC is deliberately withheld or misstated, then an unethical deception occurs. Failure to disclose information that might lead a patient to choose a different method of treatment is generally considered to be unethical.12, 13 Therefore, it seems clear to us that failure to inform patients of a possible postfertilization mechanism of an OC is a failure to provide informed consent.
PROVIDING INFORMED CONSENT
Many reproductive scientists have defined pregnancy as occurring at the point of or at some point after implantation.16, 91, 92 However, this definition does not change the fact that some patients, for personal, scientific, moral, or religious reasons, identify the start of human life at fertilization. For such patients, a form of contraception that allows fertilization and then causes loss of the preembryo or embryo may be unacceptable. Regardless of the personal beliefs of the physician or provider about the mechanism of OCs, it is important that patients have information relevant to their own beliefs and value systems.
However, the objective presentation of the potential for postfertilization effects of OCs may be complex; there are a variety of potential interpretations of the postfertilization effects depending on which aspect is emphasized: (1) One could state that OCs may significantly reduce the absolute risk per woman-year of any possible postfertilization loss in the same way that they reduce the absolute clinical pregnancy rate.78 For some women or medical personnel who believe that human life begins at fertilization, this view might render OCs, even with postfertilization loss, morally acceptable. (2) One could emphasize that once fertilization has occurred, OCs may cause at least an occasional postfertilization loss, regardless of the rate of fertilization. For some women or medical personnel who believe that human life begins at fertilization, the view that any postfertilization loss could be attributed to the effects of OCs and therefore could be considered induced rather than natural may render OCs morally unacceptable to use, even if the absolute frequency of such an event is very low.
Medical colleagues have suggested to us that postfertilization loss attributed to OCs would not need to be included in informed consent until it is either definitely proven to exist or proven to be a common event. However, rare but important events are an essential part of other informed consent discussions in medicine, primarily when the rare possibility would be judged by the patient to be important. For example, anesthesia-related deaths are extremely rare for elective surgery (<1:25,000 cases); nevertheless, it is considered appropriate and legally necessary to discuss this rare possibility with patients before such surgery because the possibility of death is so important. Therefore, for women to whom the induced loss of a preembryo or embryo is important, failure to discuss this possibility, even if the possibility is judged to be remote, would be a failure of informed consent. Others feel that an overemphasis of possible postfertilization effects might make women choose a less-effective method of contraception and therefore increase the incidence of unplanned pregnancy. Both of these views fail to acknowledge the value of a woman’s autonomy in making decisions based on informed consent. During informed consent discussions, overemphasis of any single possible risk may not result in appropriate informed consent; however, neither does choosing to not mention the possible risk result in adequate informed consent. Therefore, discussion of this potential risk should occur and should be kept within the perspective of the available medical evidence.
One possible approach to this complex issue might be to inquire of the patient whether she desires this information. The physician or provider might say, for example: “Most of the time, the pill acts by preventing an egg from forming. This prevents pregnancy. However, women on the pill can still sometimes get pregnant. Some doctors think that the pill may cause the loss of some of these pregnancies very early in the pregnancy, before you would even know you were pregnant. Would knowing more about this possibility be important to you in your decision about whether to use the pill?”
If the answer is yes, further explanation of the issues would be indicated and should occur in terms that are as understandable as possible. Proper informed consent requires patient and physician comprehension of information, the disclosure of this information, and the sharing of interpretations.14, 15 If any mechanism of any OC violates the morals of any particular woman, the failure of the physician or care provider to disclose this information would effectively eliminate the likelihood that the woman’s consent was truly informed13, 14, 93 and would seriously jeopardize her autonomy.13
Furthermore, there is a potential for negative psychological impact on women who believe human life begins at fertilization, who have not been given informed consent about OCs, and who later learn of the potential for postfertilization effects of OCs.94 The responses to this could include disappointment, anger, guilt, sadness, anger, rage, depression, or a sense of having been violated by the provider.5,/ Further research is necessary to identify the exact frequency of postfertilization effects of OCs.
CONCLUSIONS
The available evidence supports the hypothesis that when ovulation and fertilization occur in women taking OCs, postfertilization effects are operative on occasion to prevent clinically recognized pregnancy. Physicians should understand and respect the beliefs of patients who consider human life to be present and valuable from the moment of fertilization. Since it would be difficult to predict which patients might object to being given an OC if they were aware of possible postfertilization effects, mentioning the potential for postfertilization effects of OCs to all patients and providing detailed information about the evidence to those who request it is necessary for adequate informed consent.
Author/Article Information
From the Department of Family Medicine, University of South Florida, Kissimmee (Dr Larimore), and Department of Family and Preventive Medicine, University of Utah, Salt Lake City (Dr Stanford).
Reprints: Joseph B. Stanford, MD, MSPH, Department of Family and Preventive Medicine, University of Utah, 50 North Medical Dr, Salt Lake City, UT 84132 (e-mail: jstanford@dfpm.utah.edu).
Accepted for publication March 18, 1999.
We thank John R. Hartman, MD, Chris Kahlenborn, MD, G. Gayle Stephens, MD, William Toffler, MD, and Randy Alcorn, MS, for their help with conceptual development of this article and for identifying important references.
http://www.polycarp.org/larimore_stanford.htm
Based on the research of A. Glissant, J de Mouson, and R. Frydman, “Ultrasound Study of the Endometrium During In Vitro Fertilization Cycles,” the following chart was completed: